More than four years since Covid-19 was declared a pandemic by the WHO (World Health Organization) in March 2020, fear of another mass outbreak looms large. The WHO, on August 14, declared the current upsurge of Mpox or Monkeypox in Central Africa as a global emergency requiring urgent action. The global concern for the virus grew as it spread to other African countries, and, within no time, the deadly strain of Mpox – Clade 1b – crossed the African continent to reach Sweden, Pakistan, and other countries.
The virus has killed more than 500 people so far, mainly in the Democratic Republic of Congo, where the disease has been spreading since last year. The country saw more than 96% of the world’s roughly 17,000 recorded cases of Mpox this year.
Though India has not reported any cases yet, the Central government is keeping a close eye on the situation. Our healthcare infrastructure faced severe challenges during the Covid-19 pandemic, which resulted in thousands of deaths. One wouldn’t wish to be caught unawares this time.
Is Mpox As Dangerous As Covid-19 Or Swine Flu?
Mpox is a zoonotic infection that causes flu-like symptoms and skin lesions. Fatal in some cases, the WHO first declared it a global emergency in 2022.
Mpox virus can be categorised into two clades: Clade 1 and Clade 2. The first, which is found mainly in Central African countries, is more severe and has a high mortality rate. Clade 2 has milder symptoms and is found in western Africa. The latter caused a public health emergency in 2022, wherein some 300 cases — though mild — were reported from Sweden. This time, it’s the newer and more serious Clade 1b, identified in September last year, that has been driving the current outbreak.
Though experts worry that Mpox may be as dangerous as Covid-19 or the swine flu, there is a difference in the nature of transmission. Both Covid-19 and swine flu were highly infectious because they were airborne. In contrast, Mpox is transmitted through close skin-to-skin contact, talking or breathing close to an infected person, or using their soiled clothes or bedsheets. “Mpox is unlikely to become a pandemic like Covid-19 primarily due to its mode of spread. It requires very close and physical contact, unlike the airborne SARS-CoV-2. Also, symptoms like blisters on the skin are more visible indicators and therefore, it’s easier to identify the disease and isolate a person to contain the spread,” says Rakesh K. Mishra, former director of the Centre for Cellular and Molecular Biology.
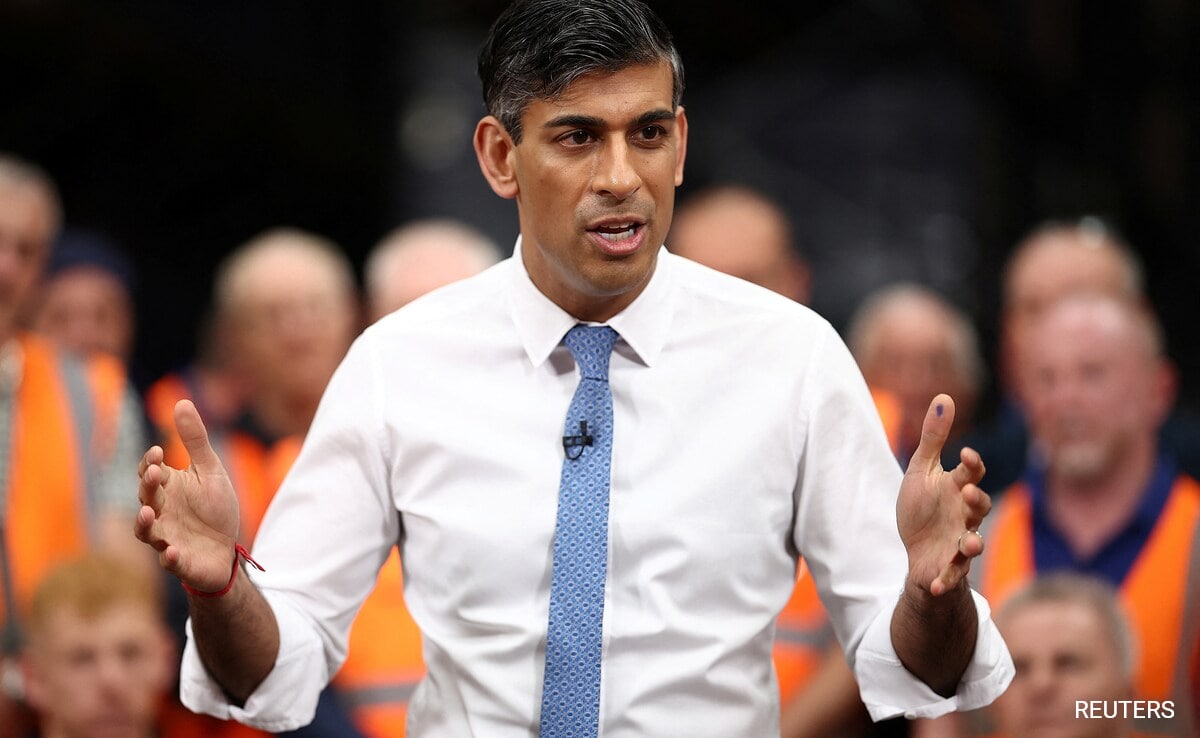
India’s first Mpox case was recorded in Kerala in 2022, from a traveller from the UAE. Soon, the virus spread within the country, with cases emerging in Delhi even from individuals who had no recent international travel. India reported 27 confirmed cases and one death that year, according to WHO. The last case in the country was in March this year, in Kerala, and since then, no new cases have been recorded.
How To Stay Safe
In response to the WHO’s warning, both Central and state governments have sprung into action. There are monkeypox advisories in place and public health measures are being taken. Both the Indian Council of Medical Research (ICMR) and the National Centre for Disease Control (NCDC) are closely monitoring the situation and reviewing international trends.
In Tamil Nadu, the Directorate of Public Health and Preventive Medicine (DPH) has already issued alerts. Reports say that passengers arriving from the Democratic Republic of Congo and Central African countries are being tracked by airport health officers and port health personnel. Both Hyderabad and New Delhi — cities popular among African students pursuing higher education — have also been placed on high alert.
The Need For Vaccines
The first Mpox strain was isolated by ICMR researchers in 2022. Pharmaceutical companies and drug manufacturers are being called upon to develop vaccines and testing kits for the virus. Existing vaccines for smallpox and chickenpox might also offer protection in India.
About other prevention strategies, Mishra says, “It is important to closely monitor the spread of the disease in different countries and be ready for screening by already available methods of DNA-based diagnostics. There is an effective vaccine already available but supply of that may not be easy to ensure.”
“Simple practices like avoiding close physical contact with suspected/potentially infected person, maintaining distance from people with symptoms, and wearing a mask, should be effective in containing the spread of the infection,” Mishra adds.
Developed nations, mostly those in Europe, already have vaccines available for those at greater risk of monkeypox. And given the high quality of healthcare there, containing the disease will be less challenging. It’s underdeveloped African countries, which have neither vaccines nor the resources to buy them, that remain at most risk and which need the most help.
(Bharti Mishra Nath is Contributing Editor, NDTV)
Disclaimer: These are the personal opinions of the author
Waiting for response to load…