This is part I of a two-part story on the virus that caused the Great Influenza epidemic. Read part II here.
In August 1997, the members of the village council of a small settlement in Alaska, called Brevig Mission, were faced with a peculiar request. A man named Johan Hultin wanted their permission to exhume a nearly 80-year-old mass grave. He claimed that he had done it before, 46 years earlier, and that he was back because his previous mission had failed.
The council gave him its blessing when its members heard what he was after. According to him, hidden beneath the frozen ground lay preserved the recipe to make the deadliest virus humankind had ever encountered.
A virus from scratch
Scientists routinely engineer new viruses in the laboratory. They make changes to the genetic material (DNA or RNA) of existing viruses to create new variants that may or may not exist naturally. Doing so allows scientists to compare the properties of the edited variants to their natural counterparts and infer the role of the changes that they made.
For example, if they observe that some patients have a higher viral load in their blood for a given disease, and a particular mutation is observed in the DNA of viruses isolated from those patients, they can introduce that mutation into the DNA of viruses that don’t naturally harbour it, to see if it improves the viral output in the laboratory.
But while scientists can easily introduce changes to the genetic material of a virus, they can’t create a virus from scratch. They have to rely on nature to do this.
So, scientists take samples from patients, make more copies of the genetic material using a technique called a polymerase chain reaction, and use it to understand the sequence of bases that makeup its genetic material. Once they have the sequence, they can tweak it.
Meet H and N
In 1995, molecular pathologist Jeffery Taubenberger, who was working on the influenza virus, was trying to understand why some strains of the virus caused pandemics while others didn’t. Taubenberger realised that in order to do that, he needed to know the genetic makeup of the deadliest strain of influenza that had ever infected humans: the virus responsible for the 1918 disaster.
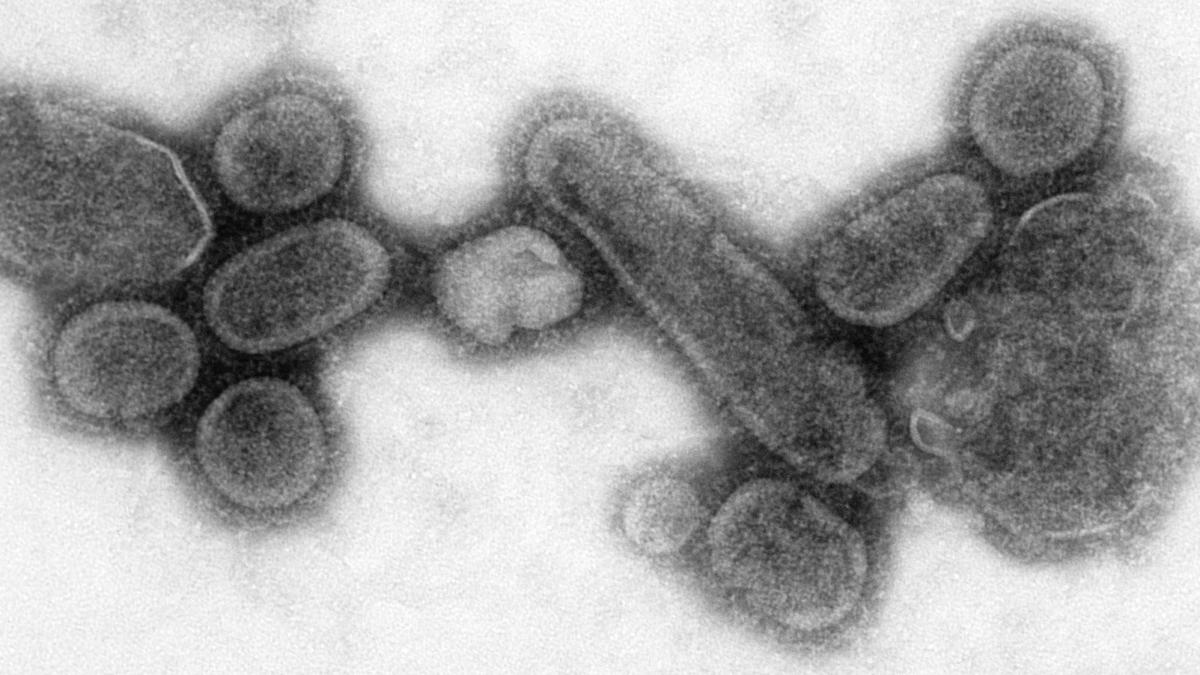
At the time, 105 years ago today, the virus was estimated to have infected 500 million people – a third of the worlds’ population then. It was notorious for its ability to cause severe disease in people aged 15-34. It has been estimated that 50 million people died as a result. (To compare, the COVID-19 pandemic is thought to have caused around 6.9 million deaths.)
Researchers designate influenza strains using the types of two genes that the virus contains, named haemagglutinin and neuraminidase, designated ‘H’ and ‘N’. There are 18 subtypes of haemagglutinin, labelled H1-H18, and 11 types of neuraminidase, N1-N11, in nature. An influenza virus contains one of each and is classified accordingly.
For example, the 1918 flu was caused by the H1N1 variant; the 1957 Asian flu was caused by H2N2; and the 1968 Hong Kong flu was caused by H3N2. There exist further sub-variations of these primary classifications, where different mutations exist in the ‘H’ and ‘N’ genes and which can further modify a virus’s properties. The 1918 flu and the 2009 swine flu were both caused by H1N1 – but they varied in disease severity due to the presence of changes on the H1 and N1 genes.
Taubenberger wanted the 1918 version of H1N1. But there was a problem. The virus had vanished after 1920, when the pandemic ended. While there were subsequent influenza outbreaks later in 1957, 1968, and 1977, those viruses were different and nowhere near as deadly as the 1918 strain. Taubenberger was adamant to use the worst of all influenza variants in his studies because studying that strain was imperative, he believed, to understanding influenza.
A letter from Johan Hultin
With great difficulty, he obtained the preserved lung samples of a soldier who had died of the disease in 1918, and extracted a small portion of the genetic material of the virus. However, because he was running out of starting material, Taubenberger couldn’t generate the complete RNA sequence. So, together with another scientist named Ann Reid, he ended up publishing a small part of the sequence in March 1997.
A few months later, Taubenberger received a letter from a doctor named Johan Hultin, who had read his article, and offered a solution to his small sample problem. Dr. Hultin claimed that in a small ocean-side village in Alaska, called Brevig Mission, there existed a mass grave in which 72 people who had all died due to the Great Influenza epidemic in 1918 had been buried. The Alaskan permafrost would have ensured the bodies were preserved almost perfectly – along with the virus.
Dr. Hultin continued that he had visited the site in 1951 and had brought a few samples back. But due to the long return journey, the samples began to thaw, and he had to refreeze them with carbon dioxide from a fire extinguisher. But despite his best efforts, he couldn’t protect them, and the multiple freeze-thaw cycles destroyed the samples.
Over a telephone call, Dr. Hultin offered to go back to Brevig Mission to retrieve more samples at his own expense. Taubenberger agreed.
Full genetic sequence
And so, in August 1997, Johan Hultin, at the age of 72, went back to Brevig Mission to finish what he set out to do as a young graduate student 46 years earlier – to get the deadly 1918 H1N1 influenza virus. The task ahead of him was fraught with the risk of him contracting the deadly virus, and almost certain death after. But neither that nor the lack of specialised equipment proved to be a deterrent for Dr. Hultin. He went ahead with his mission just the same.
The samples he brought back allowed Taubenberger and Reid to determine the virus’s full genetic sequence. The sequence allowed other scientists to unearth insights into the virus’s beginnings. It appeared to have an ancestor that was avian in origin. But there were also tell-tale signs that the virus had adapted, by evolving, to infect mammals.
In other words, the ancestral virus that infected birds had switched to infecting humans or swine. It had also been circulating for a few years, getting better at its job, before it vanished. Sometime later, it reemerged as one of the deadliest pathogens ever to afflict humankind.
But for all these remarkable insights, the virus’s genetic sequence revealed nothing dramatic about the virus itself. It failed to explain how it could infect people so quickly or why it killed millions. There were minor variations in the genetic material but this is to be expected for RNA viruses. There remained but one way to answer that question: to recreate the virus itself.
Read part II here.
Arun Panchapakesan is an assistant professor at the Y.R. Gaithonde Centre for AIDS Research and Education, Chennai.