Orange-red in colour and native to Tanzania, the Naja pallida — the red spitting cobra — is a formidable, 1.2-metre-long foe. When threatened, it raises its hood and hisses loudly. If this display doesn’t deter its predator, it opens its mouth. Muscles around the snake’s venom glands squeeze, releasing jets of venom onto the eyes, nose, and mouth of the threat. As the victim’s face sears in pain, the cobra takes the opportunity to lunge forward and bite, delivering a massive quantity of venom into the victim’s body.
The venom attacks cells in the body and damages the nervous system. For most of the cobra’s regular victims — toads, frogs, birds, and other snakes — the only fate is death. A lucky human might be spared but with a permanent disability.
Bad deal on antivenoms
Encounters with venomous snakes kill about 1.4 lakh people every year, especially in the tropical regions of Africa and Asia. Despite this alarming number, the treatment for snakebites has remained archaic.
Based on the work of French scientists in the late 1800s, antivenom is made today by injecting domestic animals like horses and sheep with small amounts of snake venom. This kicks the animal’s immune system into action, producing antibodies to neutralise the venom. Researchers extract these antibodies from the animal’s blood and transport them in cold storage to hospitals, where they are injected into the bodies of snakebite victims.
Difficulties in production, storage, transportation, and administration aside, antivenoms are also expensive and can have severe side effects in humans; some of them could be fatal.
That may soon change. In a July 2024 study published in the journal Science Translational Medicine, a team of Australian, British, Canadian, and Costa Rican scientists have reported that tinzaparin, a drug commonly used to prevent blood clots, significantly reduces damage to cells due to spitting cobra venom. The team also found the drug could reduce skin damage in mice injected with the venom.
According to a press release, the scientists have filed for a patent and may start human clinical trials soon.
According to Kartik Sunagar, an associate professor at the Centre for Ecological Sciences, Indian Institute of Science (IISc), Bengaluru, who studies the evolution of snake venoms and advanced snakebite medicines, “This discovery could pave the way for a real-world solution for regions that suffer the highest burden of snakebite morbidity.”
How venom kills cells
The venom of the red- and the black-necked spitting cobras — the two species whose venom the researchers used in the study — is “poorly understood,” R.N.V. Krishna Deepak, who studies snake venoms using computational methods at Azim Premji University, Bengaluru, said.
Our understanding of how these venoms kill human cells is worse, which contributes to the lack of advances in antivenom development.
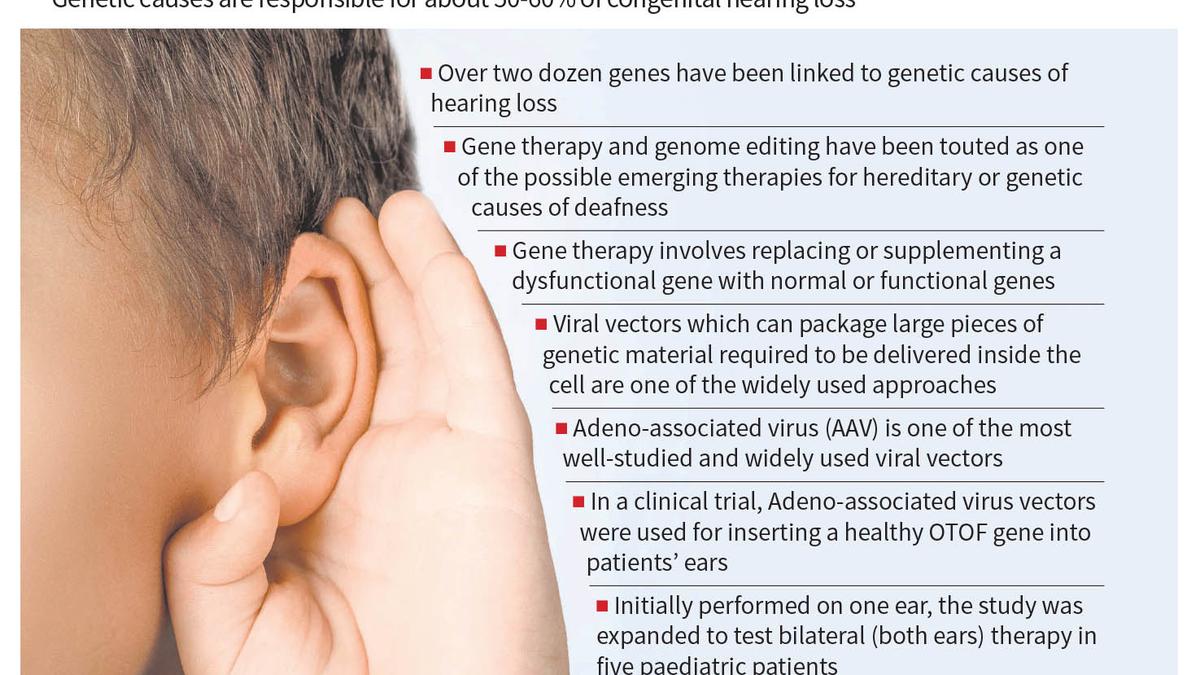
To address this issue, the researchers first investigated how spitting cobra venom affects human cells. They grew a collection of human cells in the laboratory; each member of this collection had a single gene removed. (They used CRISPR-Cas9, a Nobel-winning genome-editing tool, to build this collection.) When a gene is knocked out, cells are unable to manufacture a particular protein.
The researchers then treated this collection with the venom of either of the two snakes and selected cells that survived. Given that this resistance to spitting cobra venom had been conferred by the absence of a gene, the authors concluded the said genes were involved in facilitating the venom’s effects on normal human cells.
Further investigation revealed that many of these genes were involved in the synthesis of a sugar compound called heparan sulphate, which is known to regulate the formation of blood vessels and clots in the human body.
Blood thinner to antidote
The researchers hypothesised that if the venom’s toxicity depended on the biological pathway that synthesised heparan sulphate, artificially stopping this pathway could ameliorate the venom’s toxic effects.
One way of doing so is to introduce molecules that closely resemble heparan sulphate. As the body senses an excess of these molecules, it shuts down the pathways responsible for heparan sulphate synthesis. One such molecule is tinzaparin, a drug used to treat serious blood clots.
When the team introduced tinzaparin immediately after subjecting cells to the snake venom, the cells survived. Tinzaparin could protect these cells even when it was introduced an hour after the cells had been exposed to the venom. Further experiments revealed that tinzaparin worked by blocking the interaction between the venom and its receptor in the cell by binding to venom molecules.
When the researchers injected mice with venom from either of the two cobras along with tinzaparin, they found that skin damage resulting from the venom was much less when the mice were provided with the drug versus when they were deprived of it.
‘Hiding right under our noses’
Dr. Deepak, the Azim Premji University biologist, said the study’s use of the “highly efficient CRISPR approach” to a “mighty but neglected problem” could potentially renew the interest of the global scientific community to better understand mechanisms underlying snake venom toxicity.
The IISc’s Dr. Sunagar added that the study is “one of the few research undertakings where the molecular mechanism of how venom causes damage is taken into account to design a targeted therapy.” The therapeutic agent itself that the study proposes — tinzaparin — is inexpensive, widely available, and has been “hiding right under our noses”, Dr. Deepak said.
He added that he is excited to see how different research groups follow up on the study’s findings. In the meanwhile, he hoped the study would garner enough attention to make a case to increase funding that will allow researchers to employ “advanced and precise technologies like CRISPR-Cas9 to address the molecular mechanisms behind snakebite envenoming.”
Sayantan Datta is a science journalist and a faculty member at Krea University. They tweet at @queersprings.