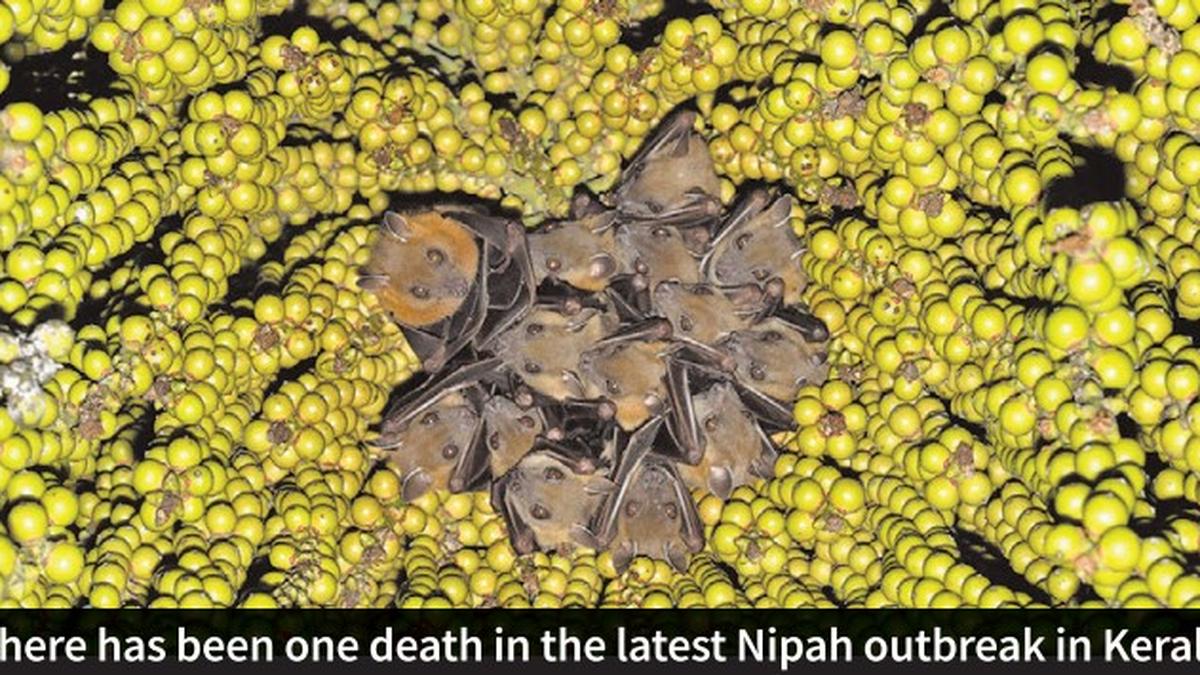
When highly pathogenic virus outbreaks such as Nipah take place, contact tracing and isolation of close contacts become critical to contain the virus spread. Public health responses can begin only when samples are tested quickly.
In a marked departure from earlier four Nipah virus outbreaks in Kerala, on July 20, samples for Nipah testing were sent to NIV Pune and also to the State government’s Institute of Advanced Virology (IAV) in Thiruvananthapuram. The Institute of Advanced Virology, which became fully functional in 2022, tested the sample in four hours and conveyed the Nipah positive test result to the health department by 9 am. Kerala waited till evening for Nipah virus confirmation by the National Institute of Virology (NIV), Pune before making an official announcement of the outbreak.
Even before Nipah was confirmed by NIV, Kerala swung into action to prevent virus spread based on the result from the IAV lab — it set up a control room in Malappuram, the epicentre of the latest outbreak, put in place a 30-bed isolation ward at the government medical college hospital in Manjeri, and imposed travel restrictions in two panchayats. Also, the Nipah patient’s route map was published on July 20 night.
Last year, Kerala was permitted to undertake Nipah testing on its own only on September 20, 11 days after the outbreak began and after 323 samples were tested for the virus by NIV. In the latest outbreak, besides the index case, the Institute of Advanced Virology has been testing all the samples of close contacts. In each case, the testing was completed in four hours and the State government was notified immediately. In contrast, it takes about 24 hours to know the result when samples are sent to NIV.
The Institute of Advanced Virology is a BSL-2 facility and follows BSL-3 practices. For Nipah, the lab has a class-3 biosafety cabinet that has an enclosed 100% negative pressure facility, which is used for virus inactivation, says Dr. E. Sreekumar, Director of IAV. A BSL-3 facility is needed only when the virus is isolated, cultured and tested on animals, and not for Nipah testing. The IAV lab is equipped to test 83 viruses, including Nipah, Zika, Chandrapura virus and influenza. “In a single sample, we carry out 30-35 tests so we are able to identify the pathogen,” says Dr. Sreekumar.
“Contrary to many outbreaks where diagnosis and confirmation have been delayed due to the requirement to ship samples to NIV, as in the case of many of the ongoing outbreaks in multiple States, the decentralised model as seen in Kerala can enable quick response to emerging pathogens,” says Dr. Vinod Scaria, a senior consultant at the Vishwanath Cancer Care Foundation. Considering the frequent outbreaks, testing and genome sequencing of emerging diseases need to be decentralised at the State level and excessive reliance on NIV has to end to enable quicker public health responses.
The importance of decentralised testing was brought to the fore recently in Gujarat that had sent samples to NIV Pune following the outbreak of acute encephalitis in children and yet remained clueless about the cause of deaths in many cases. Three weeks into the outbreak, the Gujarat government on July 18 decided to instead send the samples to the Gandhinagar-based Gujarat Biotechnology Research Centre, which is equipped with a BSL-2 lab facility to carry out whole genome sequencing to identify the virus that is causing the deaths, Ahmedabad Mirror reported. Similarly, as NIV was overwhelmed with Zika samples, the Pune Municipal Corporation in early July was considering sending samples to BJ Medical College in Pune for quicker test results.
Genome sequencing
Not only has Kerala’s Institute of Advanced Virology taken the lead in Nipah testing, it has for the first time carried out partial sequencing of the Nipah virus genome. “We carried out partial sequencing of the F and G protein coding regions [of the Nipah virus]. The coding regions showed complete conservation (both nucleotide and amino acid level) with previously reported strains from the region,” says Dr. Sreekumar. Establishing the relatedness of the virus with previous outbreaks has enabled molecular epidemiology, says Dr. Scaria. IAV will soon be undertaking whole genome sequencing of the virus. Currently, annotation of the partial genome sequence is being undertaken, and IAV intends to make the genome data publicly accessible as soon as the annotation is completed.
In the last couple of months, there have been many outbreaks — H5N1 and Zika in multiple States, the Chandipura virus outbreak in Gujarat, and Nipah outbreak in Kerala. Although many samples of these viruses have been tested positive by NIV, no genome sequence of any of these viruses are available in the public domain yet. In the case of Nipah, since the first outbreak in 2018, genome sequences were made publicly available by NIV after a delay of 6-12 months. Similar delays in positing the genome data were seen in the case of Zika samples collected from Kerala in 2021. “We have a very clear distinction between public health importance and academic imperative,” says Dr. Sreekumar about posting the genome data in a public database at the earliest.
“Delay in releasing genome sequence data significantly impacts the ability to build diagnostics, use it for understanding the introduction and genetic epidemiology apart from evolution of the pathogen, all of which are important in the public health response to an outbreak,” says Dr. Scaria.