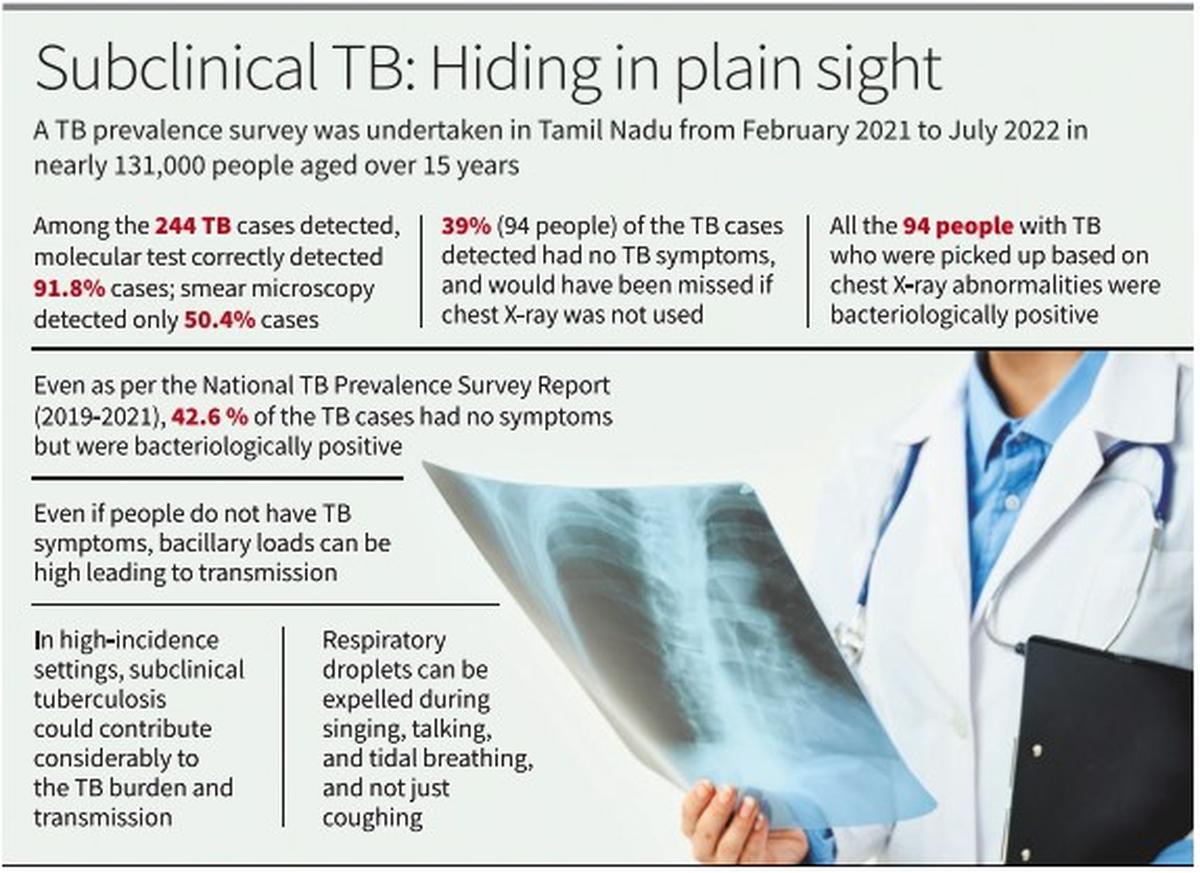
The first-of-its-kind TB prevalence cross-sectional survey was carried out among individuals aged older than 15 years across Tamil Nadu from February 2021 to July 2022. Based on the survey findings, the authors of the study from the National Institute for Research in Tuberculosis (ICMR-NIRT), Chennai have recommended that the State TB programme should prioritise the use of chest X-rays for earlier detection of cases and to cut the transmission chain, and should upscale molecular tests to increase the yield. The results were published recently in The International Journal of Tuberculosis and Lung Disease.
In a cross-sectional survey, 130,932 participants consented to participate. Among them, 130,914 underwent symptom screening and 125,870 underwent both symptom screening and chest X-ray examination. Those with symptoms of TB and/or abnormal chest X-rays were tested for TB using Xpert, smear microscopy, and liquid culture. The survey identified 244 microbiologically confirmed TB cases. Among the 244 patients with TB, only 54.5% (133 people) reported having symptoms of TB, while 92.6% (224 people) had chest X-ray abnormalities.
Among the 244 TB cases detected, molecular test (CBNAAT) correctly detected 224 (91.8%) cases, while smear microscopy was able to detect only 123 (50.40%) cases. Even among the 115 symptomatic TB cases, 89% (102) were diagnosed by CBNAAT compared with 58 (50%) who were diagnosed based on smear microscopy. The Tamil Nadu TB programme, which over-relies on smear microscopy, must scale up molecular tests, the authors write.
The most important finding from the survey is that 39% (94 people) of the TB cases detected had no TB symptoms, otherwise called subclinical TB, which would have been missed if a chest X-ray had not been used. All 94 people with TB, who were initially picked up based on chest X-ray abnormalities and subjected to sputum examination, were found to be bacteriologically positive, thus confirming TB disease. This highlights the importance of using chest X-ray for screening even in people who do not exhibit any symptoms. Currently, the TB programme in Tamil Nadu offers chest X-rays only for those with symptoms. Based on the survey findings, the State should prioritise the use of chest X-rays for earlier case detection and increase the yield.

Even active case finding of high-risk/vulnerable groups across India screens people for presumptive TB symptoms/signs, leaving out a huge chunk of people with subclinical TB. As per the India TB Report 2022, 22.1 crore individuals in India were screened for presumptive TB as part of active case-finding. Of these, only 48,329 (2.5%) were diagnosed, resulting in a low yield of just 22 per 100,000 population. Considering that TB incidence in 2022 was 199 per 100,000, active case finding, which is a targeted approach to find more cases in vulnerable populations, should have produced a higher yield. The use of chest X-ray as a preliminary screening tool along with molecular diagnostics will surely help in better detection of cases.
That 39% of TB cases detected had no symptoms is not surprising. As per the National TB Prevalence Survey report (2019-2021), 42.6 % of the TB cases, which were bacteriologically positive but did not exhibit any TB symptoms, would have been missed if chest X-ray was not included as an additional screening tool.
Besides, picking up more people with TB when chest X-ray is used, early detection of subclinical TB cases will greatly help in cutting the transmission chain. According to a March 2024 paper in the journal Lancet Infectious Diseases, a meta-analysis of surveys from a few high TB-burden countries found 27.7% of people with TB had no TB symptoms. The paper says that the majority of people with pulmonary TB in the community do not cough. “A quarter of those not reporting any cough have positive sputum smears, suggesting infectiousness. In high-incidence settings, subclinical tuberculosis could contribute considerably to the tuberculosis burden and transmission,” the paper says. In India and other high-burden countries, subclinical TB may be hiding a higher prevalence of the disease.

Even when people do not exhibit symptoms, they can still have the high bacillary loads typically associated with transmission, according to a 2021 paper in the American Journal of Respiratory and Critical Care Medicine. It also says that though cough is associated with higher infectiousness, cough is not necessary for transmission. “Subclinical TB can potentially drive a substantial fraction of transmission on a population level because of its high prevalence and long duration,” it says. Although cough expels large quantities of droplets leading to increased transmission risk, respiratory droplets can also be expelled without cough such as during singing, talking, and tidal breathing, the paper says.
Across the globe, TB incidence has been dropping more slowly compared with TB deaths suggesting that all TB measures have been less effective in stopping transmission. According to the 2021 paper, one explanation for the slower reduction of TB incidence might be that people with “subclinical TB may be the source of a large fraction of ongoing TB transmission”.